No products in the basket.
In conversation with Anna Park
I first met Anna through the dementia care awards, when I was one of the judges and she was representing one of the shortlisted companies. Impressed by her passion and drive, I started to follow Anna on Twitter, and soon saw how she brings that same passion and drive to the wide range of issues that she cares about, whether it’s nature, dementia care or circle dancing!
So I’m delighted that Anna is now working with us to improve people’s experience of care, and I’m sure you’ll find her comments and observations here as insightful and thought-provoking as I did.
What first drew you to the world of care?
I think it has to be said that experiencing a vicarage childhood meant care homes, hospitals and hospices were familiar places to me from an early age. This no doubt gave me an understanding of life’s challenges, an ability to sit and talk to anyone and a determination to always try and see the person and listen to their stories rather than focus on appearances or diagnoses.
During my degree, I had a wonderful placement teaching in a special school and a summer volunteering in a day centre for young adults with learning disabilities. I had fully expected to train as an English teacher and specialise in SEN but these experiences and a temporary position working in a Mencap group home changed my direction and shaped my understanding of what person-centred care could and shouldn’t look like. I realised then that there was far more needing to be done to train and support adults in care than I could achieve in the mainstream classroom.
I went on to take the position of a Day Services Social Worker in a Multi-Purpose Day Centre where I joined a fabulous team of passionate creatives who fully recognised the value and contribution of every individual. There was a clear focus on self-advocacy, accessing the arts and fulfilling individual potential. For eight years I ran sessions in collaborative song-writing, IT/magazine production, symbol/communication techniques, skills for work as well as dance and drama performances for all ages and abilities. The aim was always to support people to develop the skills and confidence to create, express themselves and fulfil long term goals.
The opportunity to install and assess the learning opportunities provided by a new interactive sensory music & coloured light system became the subject of my Post Grad study (P.G.C.P.C.E) and led to my next position as a consultant and trainer at OptiMusic and later OM Interactive. It was my work developing the Mobii interactive table that would further immerse me in the world of dementia care.
From a family viewpoint I was also being drawn into the world of care through the experiences of my grandparents, one on each side developing dementia whilst in their 80s. My Grandad’s lifeline in care was continuing to play his keyboard, having spent his whole life playing the organ for his local church. For my Grandma, a teacher, collector and keen gardener, it was important that she was surrounded by familiar objects and photos and had essential access to a garden. I continue to advocate the vital importance of fresh air and nature to anyone who will listen! The years my Mother worked as a care home relief manager also gave me an insight into the daily demands and rewards of life working in a care home.
You work / have worked with some other great organisations, can you tell us a bit more?
Yes, my work with sensory technology, from the mid 90s onwards, led to some exciting collaborations working alongside the creators of the first interactive musical light beams (OptiMusic) and then pioneering the use of interactive projection technology in dementia care (OM Interactive). I had always been passionate that music and the arts should be accessible by everyone, and my Post Graduate research evidenced the enormous benefits of using technology to give people creative control.
It has been exciting to be part of a new era in person-centred technology, I thoroughly enjoyed developing the content and purpose of the Mobii interactive table and researching its effect on people’s emotional and physical wellbeing. It was very humbling to have this work acknowledged as the Most Outstanding Product at the Dementia Care Awards in 2018.
However, my years in sensory product development have also taught me the huge importance of training, care culture and emotional intelligence. Any interactive tool relies on the skills and abilities of those using it, the more person-centred the session delivery, the greater the response. No product can be a ‘fix all’, they have to be in the right hands, our carers are still our greatest resource.
I have been very lucky to meet some incredible people in the world of dementia care. I was particularly honoured to be asked to become a Special Adviser (Learning Disability Inclusion and Technology) for NAPA last year. NAPA (The National Activity Providers Association) is a charity who do so much to support and promote the delivery of meaningful activities in care with quality resources, training & guidance, newsletters/magazines, a helpline, annual conference and a fabulous awards ceremony; recognising the skills and dedication of care staff nationally. So I was more than delighted to join the NAPA team in a voluntary capacity.
Intergenerational work and exposing ageism are areas I am particularly passionate about, there is so much we can learn and gift to one another over the life course. As a Trustee of the charity Ready Generations I’m looking forward to encouraging greater connection across all generations with innovative community projects, an intergenerational nursery in a care home and research-led investigations aiming to shift perspectives and value the contributions of everyone.
As a teacher I still enjoy piano tutoring, particularly when that means re-igniting someone’s passion for playing. I have weekly sessions with a lady who is living with vascular dementia which have been both moving and joyful for both of us. I also call ceilidhs and barn dances as Hedgerow Tipple, which for me is the perfect way to share my love of music and dance with all ages and abilities.
What is it about Mycarematters that made you agree to work with us?
I have admired your mission to improve the experience of care since we first met at the National Dementia Care Awards in 2018. Your determination to ensure the needs of your late husband were made known to all staff in his care homes and hospital resonated so strongly with me. Having also lost a close family member to a progressive disease I understood the daily challenge of ensuring care remained person-centred when speech had virtually gone. Our family experienced the same frustrations and miscommunications whilst also recognising the difficulties staff faced when vital information was locked away in a file on an office shelf.
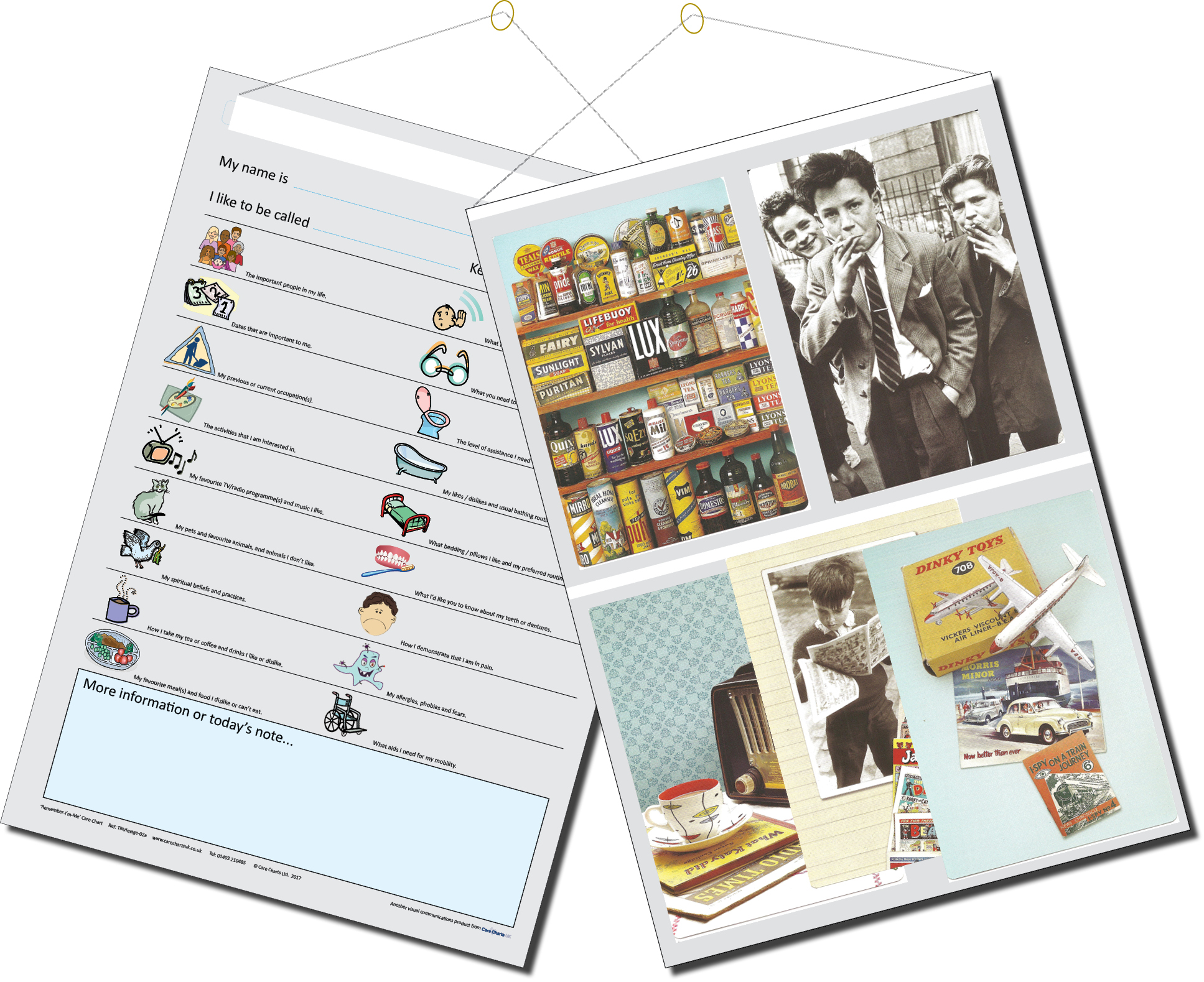
Honouring someone’s personal preferences can make the difference between a good day and a bad day. We experienced first-hand the consequences of information not being passed on with one oversight by cover staff sadly leading to a serious injury. We would certainly have used Remember-I’m-Me Care Charts if we had known about them at the time. It’s so important for all carers to have an at-a-glance snapshot of needs and preferences and for families to be reassured that what’s important for their loved ones is actively shared and understood.
I also believe that Mycarematters profiles are important for encouraging conversation and connection, a reminder to always acknowledge the person directly and explain what’s happening rather than carrying out physical care tasks in silence. As a supporter of the Butterfly Approach I believe sharing this sort of information is essential for maintaining a sense of identity and belonging. We made sure that Sarah’s O.T certificate was above her bed alongside important photos including one of her proudly completing a helicopter flying lesson. These insights help carers to see the person behind the condition and talk about things that will be meaningful for them.
More recently I have been impressed by the My Future Care Handbook, an interactive guide which we personally found useful when navigating difficult conversations with my Mother-in-law, helping us to record her care and end of life preferences. A fabulous piece of work that everyone should be encouraged to complete for peace of mind about the future!
As a not-for-profit social enterprise I admire the ethos of Mycarematters and fully support their aim to celebrate the work of other small organisations who similarly strive to improve the care experience for all. So plenty of reasons to want to join the team!
What have you got planned for Mycarematters and its customers?
Well, firstly I hope to build on the fabulous work that’s already been done by continuing to raise awareness of our social enterprise and its mission to provide solutions, training and resources to improve the experience of care.
I also plan to expand our offering by inviting partner organisations to showcase their products, guides and training resources, because there is so much good work out there that deserves a wider audience. My monthly newsletter will help to keep our customers informed of our latest additions with specialist insights and our latest news and product updates.
I’d love to see Mycarematters become a hub of excellence, a first point of call for our care providers to source reliable information and a wide variety of tried and tested tools to help them deliver person-centred care to the people they support.
I’m also very conscious that Rogers & Kitwood’s term ‘person-centred care’ is in danger of being watered down through over-use, becoming synonymous with simply ‘caring’. I think it’s vital for us to focus on what it truly means i.e. to place someone at the ‘centre’ of their care, to see the world from their viewpoint and imagine how they are feeling; to literally climb into their chair. I’m reminded of Sara Livadeas becoming a resident in a Fremantle Trust care home when she was appointed CEO. A fabulous way to try and understand how it felt to live in one of their homes.
As the newest member of the team I’m conscious that any fresh initiatives will stay true to the Mycarematters ethos, supporting people in care to always feel included, valued and their presence acknowledged, regardless of cognitive or communication difficulties.
I look forward to supporting all our customers, sharing their stories and acting on any feedback so we can continue to improve the quality of our products and services. Carers, both paid and unpaid, are doing the most incredible work everyday, they are the greatest resource of all and our aim must be to support them with the right tools and guidance to carry out their important work to the best of their ability so the caring experience is better for everyone.