Why does music have so much power? In a fascinating article the physician, neurologist and author Oliver Sacks, suggested this is a question that goes to the heart of being human. We turn to music, he said, because we need it, because of its ability to move us, to induce feelings and moods, states of mind.
We may still not know why, but those who work with people with autism or frontal lobe syndromes, and particularly with people with dementia, have recognised the power that music has to generate an emotional response, familiar music perhaps evoking memories of earlier events in people’s lives that cannot be reached any other way.
Research undertaken by the University of Iowa confirms the relevance of this for people living with dementia. UI researchers showed individuals with Alzheimer’s disease clips of sad and happy movies. Five minutes later, most were unable to recall any factual information about the films, and one person didn’t even remember watching any movies. Yet these people experienced sustained states of sadness and happiness.
The researchers concluded: “The fact that forgotten events can continue to exert a profound influence on a patient’s emotional life highlights the need for caregivers to avoid causing negative feelings and to try to induce positive feelings.”
Attempts to ensure an individual’s emotional wellbeing, therefore, should be at the heart of all care, and music is increasingly recognised as a powerful tool to assist in this aim. Of course, it has to be remembered that everyone is unique and what works for one person will not be appropriate for the next. A carer who likes nothing better than listening to hours of punk should not assume that those in their care feel the same way, equally, don’t assume that there isn’t a punk enthusiast amongst them either!
If we are looking for something to lift our mood, classical music is best, even if it’s not normally your favourite listening, according to Dr Mike Lowis. ‘In order to activate both sides of the brain, music needs to be complex so pop music and anything with a heavy beat doesn’t usually work,’ he says. (His study of peak experiences found that Wagner was more uplifting than Mozart.)
However, the inspirational and emotional story told in the American film Alive Inside, winner of the Audience Award at the 2014 Sundance Film Festival, would suggest that the true power of music is realised when particular tracks or genres are used to trigger memories and restore a sense of ‘self’, even in those with profound memory loss.
A quick story on how my husband continued to enjoy music as he neared the end of his life in a care home, rarely speaking, unable to do anything for himself, profoundly confused. As I prepared to say goodbye after one of my daily visits I asked him if he’d like any music on. He didn’t respond so I saw that a CD of one of his favourite musicians, Eric Clapton, was in the player and pressed the Play button, only to hear Geoff loudly lament “Not again!” as the sound of Clapton’s wonderful guitar playing filled the room. I had clearly not been the only lazy person in his room that day! It takes more than popping a CD into the player for music to work its magic.
Fortunately, there are a growing number of organizations, campaigns and resources dedicated to making music an integral part of dementia care. We’ve included links to some of these below.
Resources on the use of music in dementia care:
Read more about Alive Inside and the work of Music and Memory, watch the trailer and purchase the DVD here.
Organisations that offer live music experiences:
Thanks for the Memory uses the power of music to create ‘Memory Moments’ and was established by Tim Ashcroft and his wife Renee, to help those living with memory loss or dementia and to help their families. They put on concerts for those with dementia and raise money to help other groups working with dementia patients and their families.
Lost Chord is a Charity dedicated to transforming the lives of those living with dementia and their families, using music in residential homes across the UK.
Singing for the Brain is a service provided by Alzheimer’s Society.
Music in Hospitals Scotland is a registered charity and aims to improve the quality of life for people of all ages in care through the provision of professional live music. Concerts take place in hospitals, hospices, care homes, day centres and special needs schools, bringing the benefits of live music to people who need it most.
Resources for finding recorded music and creating playlists:
The Music for Dementia 2020 campaign shares best practice, research and music-based activities for people living with dementia. Their latest initiative urges people with dementia, their families and carers to build music playlists and offers free guides to help. They also offer a Musical Map for Dementia to help people with dementia find music related events and services in their area.
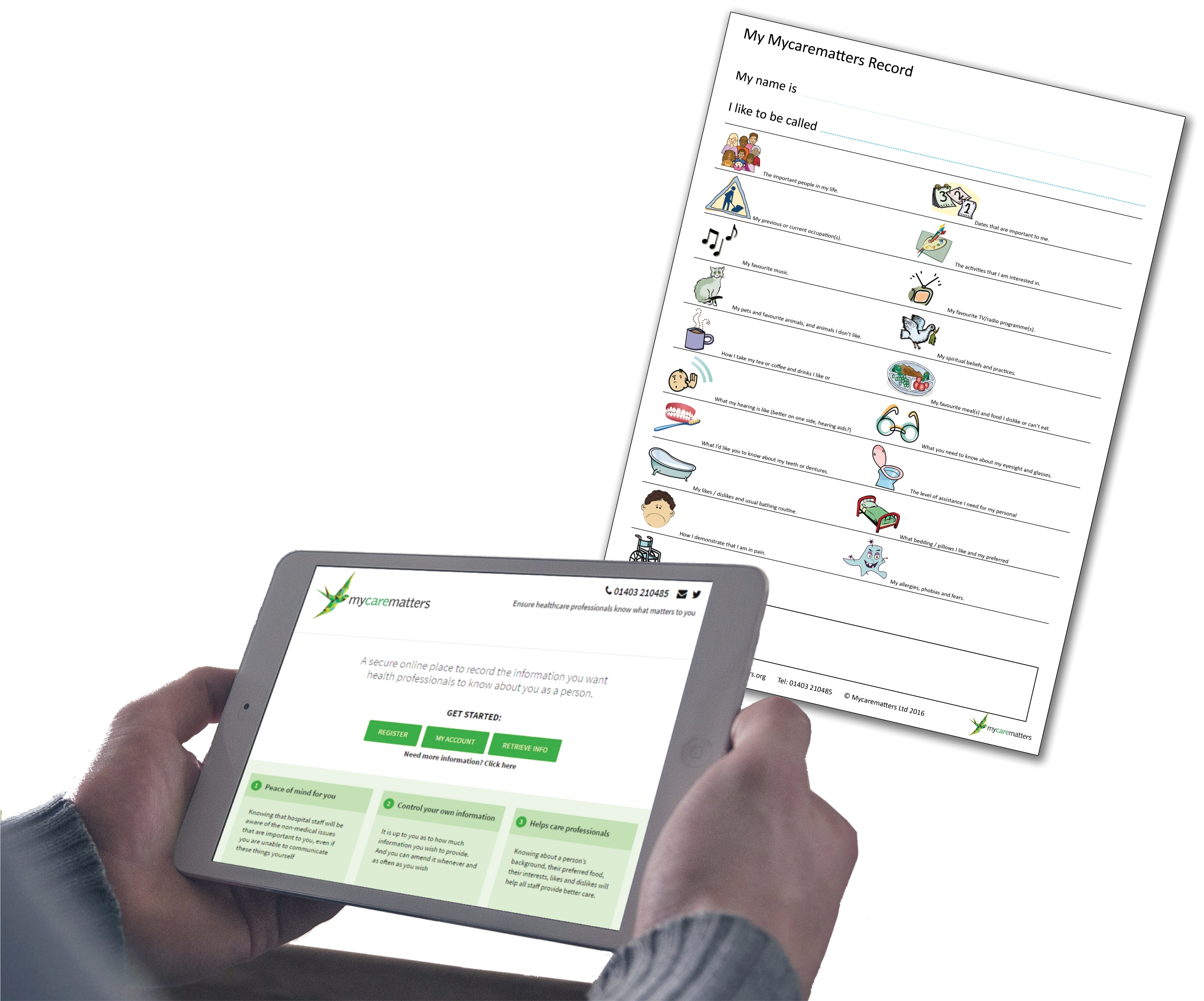
Playlist for Life has a vision: that every person with dementia has access to a unique playlist of their life, to help unlock who they are. Playlist for Life encourages families and caregivers to create a playlist of personally meaningful music on an ipod for people with dementia.
BBC Music Memories is a website designed to use music to help people with #dementia reconnect with their most powerful memories.You can use its databases to find favourite music – from classical to pop, to TV themes and even football chants – and create personal playlists.
Reminiscence Radio creates programmes featuring music from the 1940s-1970s, curated for people with short-term memory issues, designed to create a safe, reassuring place.
Information about the use and benefits of music in dementia care:
Dementia through Music: A Resource Book for Activities Providers and Care Staff, edited by Catherine Richard. An accessible guide to music activities for people with dementia for use by activity leaders, care staff and therapists, drawing on the expertise of people regularly using music in their work. Published 2020.
The British Association for Music Therapy is a good source for further information.
The fabulous infographic from 3SpiritUK, the health and social care training company, contains a wealth of information on why and how music can help in the care of people with dementia.Click here for further information
Live Music Now and the University of Winchester worked in partnership with MHA (Methodist Homes) and The Orders of St John Care Trust to investigate the impact of music on residents, staff and the general care home environment. This has led to the report “LIVE MUSIC IN CARE”, which was published in 2019. The report finds that, “Carefully delivered music can provide significant benefits for older people, care staff and care settings, contributing to person-centred care. We recommend that regular participatory music programmes be considered essential for all UK care homes.”
“Music can soothe, stimulate and bring to mind long-forgotten memories” say Age UK in their information sheet on Dementia and Music.
5 reasons why music boosts brain activity, from Alzheimers.Net
How Singing Can Help People With Dementia, from Relish.
Personal experiences and first hand accounts:
Pippa Kelly, a writer and campaigner on dementia and elderly care, often writes about music and dementia on her blog. She describes her personal experiences of witnessing the power of music to connect people even when their dementia is very advanced. She also features people, organisations and projects that enhance the lives of people with dementia and their families through music.
Full time carer for his Mum, Martyn has written about Dementia, Music and Emotions.
In this clip from Women’s Hour on Radio 4, Agnes Houston shares her personal story about music, marriage dementia and hyperacusis (a condition that affects how you perceive sounds). It’s a powerful story and highly recommended listening.
If you wish to recommend a resource for this page, please email feedback@carechartsuk.co.uk.